Large Gut Fistula Due to a Protruding Spiral Tacker After Laparoscopic Repair of a Ventral Hernia
Vishwanath Golash
ABSTRACT
Tackers (mesh fixation devices) are often used for securing the mesh in the laparoscopic repair of ventral, inguinal and hiatus hernia. By and large, their use is safe but occasionally the tackers are the cause of postoperative complications. Small gut perforations have been reported previously. We report here a case of large gut fistula secondary to an injury by a protruding tacker in the abdominal cavity presenting twenty days after the laparoscopic repair of a ventral hernia.
Submitted: 28 July 2007
Reviewed: 14 April 2008
Accepted: 21 April 2008
From the Department of Surgery, Sultan Qaboos Hospital, Salalah, Sultanate of Oman.
Address correspondence and reprint requests to: Vishwanath Golash, Sultan Qaboos Hospital, P.O.Box: 98, P.C. 211, Salalah, Sultanate of Oman. Email: haritagolash@hotmail.com
INTRODUCTION
In the laparoscopic mesh repair of ventral hernias, the mesh is usually fixed by tackers, staples or sutures. Compared to suture fixation, the mesh fixation by tacker is relatively faster and easier. For the tacker fixation to be secure, the tacker must drive all the way into the abdominal wall fascia. Depending on the thickness of the mesh, the abdominal wall and the preperitoneal fat, the tackers sometimes are not long enough to have a good hold on the fascia to secure the mesh. Improper fixation can leave a loose tacker in the abdominal cavity or a sharp protruding end giving rise to complications.
CASE REPORT
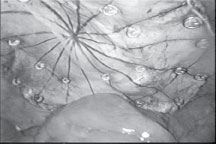
A 50 year old female patient was admitted for routine laparoscopic mesh repair of her recurrent ventral hernia. On laparoscopy, a part of the greater omentum was found inside the sac. After reducing the hernial content, the defect was repaired using a 15x15cm dual mesh plus biomaterial, (a two layered biomaterial composed entirely of polytetrafluroethylene, Gore-Tex USA). The mesh was fixed using a combination of sutures (Ethilon) and tackers {mesh fixation device, OMS-TTSD, 5mm titanium, single use instrument with 20 helical fasteners, Tyco healthcare, USA}. Her postoperative recovery was uneventful apart from a small seroma in the hernial sac and she was discharged home on third day. She presented twenty days after the surgery with a swelling and redness of the skin at the previous hernial site. On examination, infection of the seroma was suspected and some 60ml of offensive, smelling pus was aspirated. She was put empirically on broad-spectrum antibiotics and the seroma cavity was laid wide open. The cultures grew Eschericia coli and Klebsiella. The wound was irrigated several times a day in the hope of salvaging the mesh. Over the course of weeks the wound healed slowly except for a persistent sinus in the middle of the wound which continued to discharge offensive pus which on culture grew intestinal organisms. Infection of the mesh was suspected and the possibility of its removal was discussed with patient. A sinogram performed through the sinus opening showed the contrast tracking to the site of a tacker and on further injection it filled a part of the proximal transverse colon. A tacker had eroded into the colon resulting in a fistula (Figure 1, 2). A barium enema did not show the fistulous tract or a leak or any irregularity.
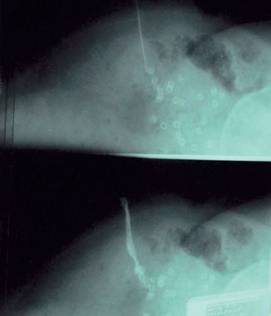
Figure 1: Sinogram showing the fistulous tract leading to the tacker.
Multiple tackers are seen at the site of fixation of mesh
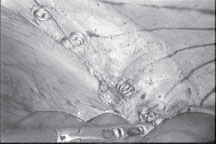
A laparotomy was performed and showed adhesions between the mesh, omentum and bowel which were separated. The sharp end of a tacker was seen eroding into the proximal part of the transverse colon (hepatic flexure) making a fistulous communication to the skin. The colon was mobilized and a limited right hemicolectomy was performed. The mesh and all the tackers were also removed. She made an uneventful recovery and was discharged. She was seen six months after the surgery and there was no recurrence of hernia or fistula.

Figure 2: Further injection of dye filling the ascending colon
DISCUSSION
The fixation of mesh in the laparoscopic repair of ventral hernia with tackers is a fairly standard technique among laparoscopic surgeons (Figure 3, 4). But there are rare reports of tacker related complications of adhesions, pain, hernia, intestinal obstruction, perforation of the bowel or urinary bladder and death. 1, 2, 3, 4 The length of a tacker is 4 mm long and depending on the thickness of tissue it may penetrate the neighboring structures with disastrous complications. If not carefully fixed these tackers could fall into the abdominal cavity or the sharp end of a tacker which is not buried properly may cause injury over a time even with normal patient movement (Figure 5, 6, 7, 8). Alternative techniques of suture fixation of mesh may avoid the tacker related complications. 5
Figure 3: Intraperitoneal Tacker fixation of mesh |
Figure 4: Helica (Spiral) tacker fixation device |
Figure 5: Intraperitoneal sharp protruding end of the spiral tacker |
Figure 6: Spiral tacker used for intraperitoneal fixation of mesh in laproscopic repair of ventral and incisional hernia |
Figure 7: A loose spiral tacker being removed
|
Figure 8: A loose spiral tacker lying on the intestines
|
REFERENCES
-
Ladurner R, Mussack T. Small bowel perforation due to protruding spiral tackers: a rare complication in laparoscopic incisional hernia repair. Surg Endosc 2004; 18:1001.
-
Patient injury or death could result from improper use of U.S. Surgical Helical Tacks, ‘Health Devices’ 2004; 8:293-295.
-
Karahasanoglu T, Onur E, Baca B, Hamzaoglu I, Pekmezci S, Boler DE, Kilic N, Altug T. Spiral tacks may contribute to intra-abdominal adhesion formation. Surg Today 2004; 34:860-864.
-
Lantis JC2nd, Schwaitzberg SD. Tack entrapment of the ilioinguinal nerve during laparoscopic hernia repair. J Laparoendosc Adv Surg tech A. 1999; 9:285-289.
-
Golash V. Laparoscopic geometrical repair of ventral hernia: how I do it. Surgeon ( Journal of Royal College of Surgeons of Edinbourgh and ireland) February 2006; 4:33-38.