Central Nervous System Aspergillosis causing Spinal Cord Compression
Faraz Ahmed,1 and Riaz Ahmed DM2
doi:10.5001/omj.2010.67
From the 1Department of Bone and Joint Surgery; 2Department of Neurology,
Sri Ramachandra Medical College, Porur Chennai-116, India.
Received: Apr 27, 2010
Accepted: May 12, 2010
Address correspondence and reprint request to: Dr. Riaz Ahmed, Department of Neurology,
Sri Ramachandra Medical College, Porur Chennai-116, India.
Email: dr.faraz@hotmail.com
Central nervous system (CNS) aspergillosis is a rare and uniformly fatal complication of disseminated disease, involving the cerebral hemispheres and cerebellum in the majority of cases. It is a ubiquitous mold and refers to a group of diseases caused by monomorphic mycelial fungi of the genus Aspergillosis fumigatus. Outbreaks of invasive aspergillosis are a problem in immunocompromized persons after they are exposed to air-borne spores.1 Aspergillosis causing spinal cord compression due to epidural abscess formation and hypertrophic pachymeningitis is a rare entity, thus such a case is presented herewith.
A 16-yrs old male was diagnosed in early childhood of chronic granulomatous disease with recurrent abscess formation of lymph nodes and pneumonias. He was on regular daily trimethoprim-sulphamethaxazole prophylaxis. At twelve years of age, he developed osteomyelitis of the right 10th rib and underwent resection and the necrotic material grew Aspergillosis fumigatus. He was treated with amphotericin infusion for three weeks followed by itraconazole for a month. Three years later, he developed progressive weakness of both legs with difficulty in walking.
Clinical examination revealed that the patient had spastic paraperesis at a D10 spinal level with spinal tenderness at D7-D9. There was no obvious swelling in the paraspinal region at that time. The bladder and bowel functions were intact although he had little hesitancy of micturation. The MRI of the thoracic spine revealed paravertebral soft tissue density in the lower dorsal region D6-D8 with liquefaction in the centre consistent with abscess. There was also a moth-eaten appearance and destruction of D7 vertebral body, (Fig. 1). Orthopedician was consulted, the abscess was drained followed by laminectomy of D6 to D11 vertebrae and decompression was performed. The abscess material grew Aspergillosis fumigatus. He was started on high-dose amphotericin B for 30 days. Later, itraconazole was given for a month. He also received broad-spectrum antibiotics, namely imipenum, ciprofloaxacin and amikacin during the postoperative period. He developed thrombophlebitis at the injection site, and later episodes of hypokalemia which were managed by potassium upplements. He was then put on plaster jacket and discharged. On reviewing him after a month, he was paraplegic with Grade 2/5 power in legs and had urinary and bowel involvement.
There was also abscess formation at the operation site with sinus, discharging pus. The wound swab grew aspergillosis and he was given a six-week course of amphotericin B and itraconazole. Bone marrow transplantation was planned but he developed persistent fever and the blood culture revealed Acenobacter. Despite treatment with many antibiotics, the patient died of septicemia.
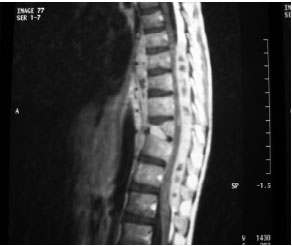
Figure 1: MRI dorsal spine -T1 weighted sagittal contrast- showing extradural aspergillosis compressing spinal cord D6-8 with collapse of D7 vert. body
CNS aspergillosis primarily affects adults. It occurs as a sino-cranial infection in all the reported cases and spinal cord involvement is either due to contiguous spread from the lungs or affecting cord prior to lungs indirectly by hematogenous route.2 Recently, there has been some increase in the incidence of invasive aspergillosis in the acquired immunocompromized individuals.3
Thus disseminated aspergillosis is a devastating disease in the immunocompromized patients and the ultimate prognosis is bad. The neurological disability was worse despite aggressive management.
-
Walmsley S, Devi S, King S, Schneider R, Richardson S, Ford-Jones
L. Invasive Aspergillus infections in a pediatric hospital: A ten-year review. Pediatr Infect Dis J 1993; 12:673-682. -
Nakazato I, Kamada Y, Taira T. Massive spinal cord necrosis associated with adult T-cell leukemia by Aspergellosis. Virchow Arch A Pathol Anat Histopathol 1993; 423:397-400.
-
Klenschmidt-DeMasters BK. Central nervous system aspergillosis: A 20 yr retrospective series. Hum Pathol 2002; 33:116-124.
How to cite this article
Ahmed F, Ahmed R. Central Nervous System Aspergillosis causing Spinal Cord Compression. OMJ 2010 July; 25(3):238-239.
How to cite this URL
Ahmed F, Ahmed R. Central Nervous System Aspergillosis causing Spinal Cord Compression. OMJ 2010 [Online] July; 25(3):238-239. Available at http://www.omjournal.org/BriefCommunication/FullText/201007/FT_CentralNervousSystem.html.