A Case of Pseudohypoaldosteronism as the Presentation of Bilateral Ectopic Ureter in an Infant
Anutosh Shee,1 Kalarikkalveetil Saieda2
Shee A, et al. OMJ. 25, 137-140 (2010); doi:10.5001/omj.2010.37
From the 1Department of Pediatrics, Mafraq Hospital, Abu Dhabi-Dubai Highway, Abu Dhabi, United Arab Emirates, 2Mafraq Hospital, Abu Dhabi, United Arab Emirates Assisstant Professor, Gulf Medical University, UAE.
Received: 06 Feb 2010
Accepted: 12 Mar 2010
Address correspondence and reprint request to: Dr. Anutosh Shee, Department of Pediatrics, Mafraq Hospital, Abu Dhabi-Dubai Highway, Abu Dhabi, United Arab Emirates.
E-mail: shee_anutosh@rediffmail.com
Shee A, et al. OMJ. 25, 137-140 (2010); doi:10.5001/omj.2010.37
Ectopic ureter occurs in only 0.025% of the population. Approximately 10% are bilateral with a 6:1 female to male ratio.1 In females, more than 80% of ectopic ureter drains duplicated systems. In males, it mostly drains a single system. In males, the ureter may terminate at the bladder neck (48%), seminal vesicle (40%), ejaculatory duct (8%), vas deferens (3%), or epididymis (0.5%). In females, the ureter may terminate at the bladder neck (35%), vestibule (30%), vagina (25%), or uterus (5%).1 When present, ectopic ureter can be associated with duplex kidneys in 85% of the cases. Clinical manifestations of this malformation include incontinence and urinary tract infections.2 Ectopic termination of the ureter is the result of the high (cranial) origin of the ureteral bud from the mesonephric duct. The delayed incorporation of the ureteral bud into the bladder results in ureteral orifice to be more caudal and medial. A sufficient tunnel length of the sub mucosal ureter is the most important component of Vesico ureteic obstruction (UVJ). Being asymptomatic, most children present with an abnormal finding on routine prenatal ultrasound. Some patients present with urinary tract infection (UTI), cyclic abdominal pain, abdominal mass, and hematuria. Other presentations include hypertension, proteinuria, or even renal insufficiency. Approximately 50% of females present with constant urinary incontinence or vaginal discharge.
A 3 months old Caucasian female was presented at the age of two months following her routine vaccination. She became lethargic and feeding poorly. She was admitted to a private hospital where her initial blood electrolytes showed subtle changes of hyponatremia and hyperkalemia, which settled following intravenous fluid infusion (0.45Nacl with 5%D). Antibiotics were initially administered empirically and discontinued at 48 hrs after negative urine culture reports. She was discharged home on the fifth day. At 3 months old, she developed similar symptoms and was admitted to the pediatrics unit, Mafraq Hospital. Her weight gain was satisfactory, but very recently her parents noticed a weight lag. She was born from non consanguineous parents by caesarean section; indication being previous sections. On the fetal anomaly scan conducted at 20 weeks of gestation, the left kidney was found to be slightly larger than the right one. But there was no follow up scan. The baby was born at term weighing 2.5 Kg. The neonatal period was uneventful. No congenital anomaly was noted. After the initial few days of breast feeding, bottle feeding was commenced. While admitted to the pediatrics unit, the patient looked lethargic. Her heart rate was 110/min, respiratory rate was 36/min and capillary refill was less than 2 seconds. She was apyrexial with mild to moderate dehydration. Her blood pressure was 113/64 and both femoral pulses were palpable. Systemic examinations were normal with normal genitalia. Serum electrolytes revealed 120meq/l of sodium and 8.4meq/l of potassium. She was resuscitated with normal saline and also received simultaneous treatment for hyperkalemia. After the initial resuscitation, her serum potassium dropped to 7.5meq/l but she remained hyponatremic (119meq/l).
There was normal anionic gap and compensated metabolic acidosis. Urinary sodium, chloride, potassium and calcium were abnormally high. All these features were denoting renal tubular acidosis type 4; relative inadequacy of serum aldosterone. Serum urea and creatinine were initially slightly raised but brisk improvement on IV fluids suggesting dehydration was the possible explanation. Her leukocyte count was 29,000/dl with neutrophil predominance; Hb was 97 gm/l, Platelets count was 250000/dl, C-reactive protein was 51 mg/l and Procalcitonine level was suggestive of systemic bacterial infection. Urinalysis showed high protein with protein creatinine ratio of 2.09. Urine was full of pus cells, and was positive for bacteria and nitrites. Serum hormone levels such as cortisol, Dyhydroepiandrosterone acetate (DHEA), adrenocorticotropic hormone (ACTH), 17-OH-progesterone, androstendione, thyroxin, all were within normal range. Her serum aldosterone level was very high (more than 2744 IU/l), confirming PHA.
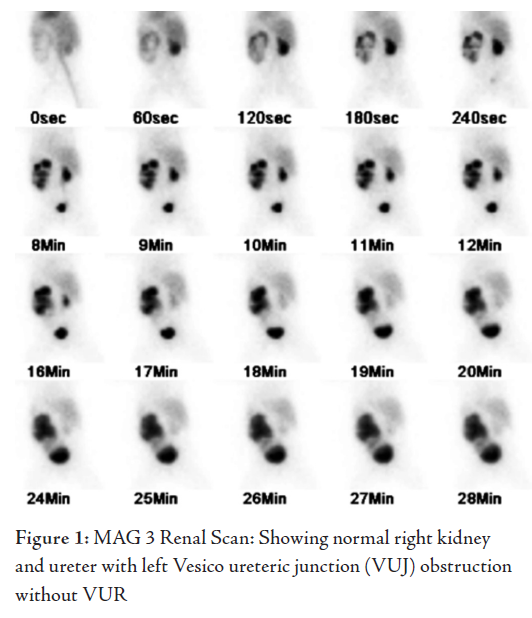
Initial renal ultrasound scan showed normal right kidney and ureter. Her left kidney was enlarged and there was grossly dilated left ureter with debris suggesting pyelonephritis. The bladder was compressed by the grossly dilated left ureter. Both the ureters were abnormally inserted to the bladder at a lower level, right one being just distal to neck of the bladder into the urethra. Surprisingly, there was no evidence of any dribbling. Intravenous cefotaxime was commenced for E-coli urinary tract infection. MAG3 scan confirmed normal functioning right kidney, moderate impairment of function of the enlarged left kidney with hydronephrotic changes, hydroureter and evidence of organic obstructive uropathy at the left VUJ with abnormal insertion to the bladder (Fig. 1). Initial management was conducted with adequate saline infusion and correcting hyperkalemia with sodium bicarbonate, salbutamol nebulisation, resonium salts and calcium infusion. Later, the patient was kept on oral sodium supplements (15 mmol per day) maintaining normal electrolytes. She underwent left ureterostomy operation to facilitate the drainage. Postoperatively, she had another episode of UTI and was treated with intravenous Meropenem. At 4 weeks follow up, her electrolytes remained normal and serum Aldosterone level resumed normal range.


The patient was then planned for reconstructive surgery for reinsertion of both ureters which was conducted after 6 months of the primary procedure.
The electrolyte imbalance presenting early in life is a matter of emergency, as life threatening conditions like congenital adrenal hyperplasia can present similarly. Congenital adrenal hyperplasia (CAH) should be considered in all neonates with hyponatremia coupled with hyperkalemia. Therefore, presumptive diagnosis of CAH was made in this case and hydrocortisone was started pending the hormonal study. The history of renal size disparity noted in the antenatal period was suggestive of renal pathology. Most structural anomalies of renal calyces noted at 20 weeks of gestation tend to be corrected spontaneously.3
The effects of urinary tract obstruction on the developing kidney depend on the time of onset, location, and degree of obstruction. Ureteral obstruction during early pregnancy results in dysplasia of the renal parenchyma and a reduction in the number of nephrons. Partial or complete ureteral obstruction in neonates causes renal vasoconstriction, glomerular hypoperfusion, impaired ipsilateral renal growth, and interstitial fibrosis. The recovery of renal function after relief of urinary tract obstruction is related to age.4 During complete ureteral obstruction, renal blood flow progressively decreases. Renal blood flow is 50% of normal after 24 hours, 30% at 6 days, 20% at 2 weeks, and 12% at 8 weeks.3 After ureteral obstruction, there is a rapid influx of macrophages and suppressor T lymphocytes in the cortex and medulla and increased urinary thromboxane A2, as well as a decrease in the glomerular filtration rate.5 The production of thromboxane A2 by the infiltrating macrophages contributes to the renal vasoconstriction and poor medullary blood flow. After the release of the obstruction, the cellular infiltration is slowly reversible, requiring several days to revert to near normal levels.5
The history of admission of the baby in another private hospital with subtle changes in electrolytes which reversed in few days of saline infusion was indicative of hypoaldosteronism. The aldosterone resistance form of RTA type IV was another possibility.
The Aldosterone resistance state, also known as PHA has been coined to describe disorders of electrolyte homeostasis characterized by a condition of renal tubular lack of sensitivity to aldosterone. There are two subtypes. Type I is a hereditary disorder related to the loss of function of the mineralocorticoid receptor. In recent years, it has become clear that type 1 PHA is a heterogeneous syndrome that includes at least two clinically and genetically distinct entities with either renal or multiple target-organ defects.6 While Type II is described as pseudohypoaldosteronism (PHA2), also recognized as Gordon’s Syndrome, it is thought to be a primary renal secretory defect that results from enhanced chloride reabsorption and consequent hyperkalemia, metabolic acidosis, and low-renin arterial hypertension. The normal serum chloride level in this patient was not in favor of this diagnosis.6
Renal PHA1 represents the most frequent form of primary PHA and is related to the loss of function of the mineralocorticoid receptor. The mode of inheritance is autosomal dominant with variable expression, although many cases appear as sporadic. The reasons for phenotype differences are unknown, but they may be related to intercurrent volume-depleting events or to dietary habits of salt ingestion during life. In addition, the coexistence of polymorphism or mutations in the gene encoding epithelial sodium channel could play a potential role.
The severity of clinical and laboratorial manifestations at the time of the diagnosis is inversely correlated to the age of the patient, ranging from a neonatal life-threatening salt wasting syndrome to an adult asymptomatic elevation of plasma aldosterone levels. In the studied case, further investigation revealed obstructive uropathy as the original cause of the type IV RTA and pseudohypoaldosteronism. Bilateral obstructive uropathy is a well known cause of RTA type IV and PHA because of insensitivity of the aldosterone to the tubules. Acute pyelonephritis in the presence of urinary tract anomalies increases the risk of PHA, although both factors independently can cause aldosterone unresponsiveness.7
Unilateral renal tubular unresponsiveness to aldosterone should not cause any electrolyte imbalance because of the normal functioning of the opposite kidney. In this case, the obstruction is unilateral in the presence of PHA, left us to two possibilities. Firstly, this may purely be a coincidence of type I PHA with a concordant association of unilateral VUJ obstruction and bilateral ectopic ureters. The second possibility was that in the presence of unilateral obstruction, there was also super added pyelonephritis, both of which were contributing together to produce transient secondary aldosterone insensitivity.
No genetic test was carried out for the PHA I and PHA II. However, as the condition disappears following the relieving the obstruction and treating the infection, it is the second possibility which is most likely.
The take-home message from this case is to appreciate the common occurrence of ureteral anomalies and the uncommon presentation of electrolyte disturbances because of the ectopic ureter. A very high index of suspicion is required to rule in or out the possibility of renal tract anomaly when there is abnormality of electrolytes in the body, particularly if it is persistent and/ or recurrent. This case identified the rare presentation of the relatively common anomalies of the human body. It is also a very good example for assurance that this hormonal change is transient and can be corrected on its own when the obstruction is relieved and infection is controlled.
ACKNOWLEDGEMENTSThe authors reported no conflict of interest and no funding was received on this work
REFRENCES
-
Husmann DA. Ureteral Ectopy, Ureteroceles, and Other Anomalies of the Distal Ureter. In: Gonzales ET, Bauer SB, eds. Pediatric Urology Practice. Philadelphia, Pa: Lippincott Williams & Wilkins;. 1999:295.
-
Mart?n MS, Garc?a-Ripoll TJ, Ru?z SA, Rodr?guez GV, Ferro RJ, del Busto FE. Ectopic ureter as cause of pyonephrosis and urinary incontinence .Actas Urol Esp. 2008 Feb; 32(2):256-260. Spanish
-
Shukla AR, Cooper J, Patel RP, Carr MC, Canning DA, Zedric SA, et al. Prenatally detected primary megaureter: a role for extended followup. J Urol. Apr 2005;173(4):1353-1356.
-
Chevalier RL: Effects of ureteral obstruction on renal growth. Semin Nephrol 1995; 15:353-360.
-
Schreiner GF, Harris KPG, Purkerson ML, Klahr S: Immunological aspects of acute ureteral obstruction: immune cell infiltrate in the kidney. Kidney Int 1988; 34:487-493.
-
Komesaroff PA, Verity K, Fuller PJ. Pseudohypoaldosteronism: molecular characterization of the mineralocorticoid receptor. J Clin Endocrinol Metab. 1994 July; 79(1):27-31.
-
Melzi ML, Guez S, Sersale G. Acute pyelonephritis as a cause of hyponatremia/ hyperkalemia in young infants with urinary tract malformations. Pediatr Infect Dis J. 1995 Jan; 14(1):56-59.